Transparency International Kenya with the support of the Health Action Fund convened a Learning Circle on Health Financing on 9th November 2018 at Heron Portico Hotel in Nairobi. The Learning Circle sought to initiate discussions on Transparency and Accountability in Kenya’s Health Financing Models with the specific topics of discussion being:
- Experience Sharing Working on Accountability in the Health Sector
- Familiarisation of participants with Kenya’s Health Financing Models
- Transparency and Accountability considerations in realising the Right to Health
- Designing Working Strategies for Health Accountability
The meeting was attended by:
- Civil Society Organisations working in the health sector specifically on governance and accountability processes including: the Kenya Legal & Ethical Issues Network (KELIN), The Institute of Social Accountability (TISA), Open Society Initiative for East Africa (OSEA), the Kenyan Section of the International Commission of Jurists (ICJ-Kenya), East African Centre for Human Rights (EACHRights), Amref Health Africa in Kenya and the Global Initiative For Economic, Social And Cultural Rights.
- Health Practitioners from the Kenya Medical Practitioners, Pharmacists and Dentists’ Union (KMPDU).
- Consultants on Economics and Health Financing.
- Community representatives attached to the Action for Transparency (A4T) project implemented by TI-Kenya.
- Project partners on the A4T project from Fojo Media Institute , a media development organisation based in Sweden.
Experience Sharing Working on Accountability in the Health Sector
Titus Gitonga a Programme Officer from TI-Kenya presented on the various interventions by the organisation noting that TI-Kenya has over the years developed innovative approaches aimed at empowering citizens with information in order to effectively participate and demand accountability within the Health Sector. Among the innovative approaches adopted include:
- The Mobile Drug Tracking System (MDTS) . MDTS is a web and mobile based platform used to track the availability and movement of drugs and pharmaceuticals at facility level. MDTS also incorporates citizen modules where information regarding availability of drugs can be accessed via location and facility and provides for a short code which allows for registration by users to get various updates regarding the drug groups.
- Another innovative approach is the Action for Transparency (A4T) A4T is a Nairobi based project aimed at empowering citizens to monitor the allocation and utilisation of funds to public primary schools and health centres. The project incorporates the use of social accountability tools such as Public Expenditure Tracking surveys and social audits to track the flow of resources at health centres and disseminate the information through web and mobile based platforms including the A4T mobile App available for android and IOS phones.

- The Health Sector has also been identified as being among the sectors highly affected by corruption. The 2017 East Africa Bribery Index (EABI) signifies that corruption in the form of bribery continues to be rife in provision of Medical and Health Services, identified as among the top ten most prevalent sectors in regard to bribery. Reporting bribery incidences also remains very low with an overwhelming majority (94%) of Kenyans who were surveyed indicating that they encountered bribery but did not report to any authority or person.
- Following a report done by TI-Kenya, KELIN and the Society for International Development, the Ethics and Anti-Corruption Commission went on to carry out a systems and procedures review of the Health Sector and also released a report titled, ‘Review of Systems, Polices, Procedures and Practices in the Pricing of Pharmaceutical and Non-Pharmaceutical Supplies in the Kenya Public Health Sector’. The EACC report among other findings highlights the systemic weaknesses and opportunities existing in the procurement and dispensing stages of pharmaceutical and non- pharmaceutical supplies in the public sector and recommends compliance with national specifications for medical and medical suppliers, disclosure of evaluation criteria in bid documents and capacity building in market survey to address noncompliance issues with national standard specifications for medical and medical suppliers in the acquisition stage.
Ms. Linda Wanjiru, a Programme Officer at KELIN familiarised participants on the work that KELIN has been doing in the Health Sector specifically in relation to governance, pushing for transparency and accountability in accessing information and demanding for compliance with existing legal provisions on access to information, public participation and prudent use of public resources. She indicated that in partnership with other organisations including TI-Kenya, Katiba Institute and ICJ-Kenya, they had submitted request for information letters to the Kenyatta National Hospital (KNH) in relation to construction of a private hospital at KNH and another to the Council of Governors seeking information on the Agreement between Kenya and the Cuban Doctors with no response as at the time of the forum.
Ms. Wanjiru also indicated that through an initiative by OSEA, KELIN is leading the Health and Governance Convening – Kenyan Chapter. The Convening aims at enhancing collaborative work between different organisations working in the Health Sector and has since formed two working committees to assist in driving the accountability agenda including: Research and Evidence Gathering Committee; and the Litigation Committee. She invited participants to join in on the Convening and be part of the work being undertaken by the various organisations already in the committee.
Mr. Aggrey Aluso, the Health Rights Program Manager at OSEA also familiarised the participants with the organisation’s work supporting the Health Convening in Kenya and other participating countries including Uganda and also indicated that they were keen on supporting governance work on open contracting and good governance in the health sector.
Mr. George Githinji working on public budgets at TISA also gave a highlight on TISA’s experience in advancing public participation in the budget process. TISA also had a learning session on Private-Public-Partnerships for which the health sector also has had some huge investments around and would thus be interested in advancing these discussions.
EACHRights and ICJ-Kenya were in the initial stages of working in the Health Sector having participated in marketisation and privatisation of the health sector discussions initiated by OSEA.
Dr. Wala Elizabeth, the programme director for health systems strengthening at Amref Health Africa also indicated that the organisation was engaged in capacity building in Nairobi, Kwale, Kisumu and Vihiga of health practitioners on a health model that ensures continuous quality improvement in the delivery of health services in county and sub-county health facilities. The Kenya Quality Model for Health (KQMH) is a systems approach to strengthening quality health care in Kenya towards universal health coverage through training and mentorship using the national health information database (DHIS2).
Kenya’s Health Financing Models
This session was moderated by Dr. Matiko Riro. Dr. Matiko is a Doctoral Fellow in Health Economics at the University of Bergen in Norway. He is a medical doctor and a Commonwealth Scholar with an MSc in Public health (Health Economics) from the London School of Hygiene & Tropical Medicine (LSHTM).

It was noted that Kenya has made a commitment of accelerating its progress to achieving Universal Health Coverage (UHC) and has taken a number of steps to reform its healthcare system, to put it on the path to realising this goal.
Currently only 17 % of Kenyan households are covered by health insurance of any type, while the rest of the population relies either on donor aid, government spending or out of pocket spending for accessing health care. This makes the ambition to provide universal quality health care to all those in need, regardless of their ability to pay, a major undertaking that will require a major shift in the mechanisms and systems through which health is governed, financed and delivered.
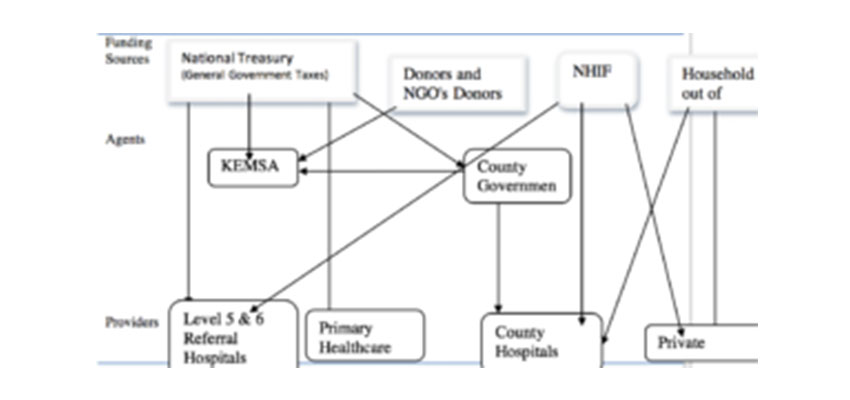
Participants discussed the diagrammatic representation on flow of funds for the health sector below:

Participants described the flow of resources in the health sector as, “Confusing”, “Complicated”, “Inconsistent”, “Unrealistic”, “Incomprehensible”, among other adjectives describing just how complicated public financial flows in the health sector has become over the years. Some of the concerns raised on transparency and accountability in health financing include:
- Lack of effective collaboration between the National and County Governments in designing effective laws, policies and guidelines for enhanced accountability on health finances;
- Appropriation of County health functions by the National Government thereby also taking up budget allocations;
- Lack of research to inform effective resource allocation and utilisation;
- Corruption through inflated procurement costs for pharmaceutical and non-pharmaceutical products, equipment’s and services;
- Unequal and inadequate distribution of health practitioners/professionals;
- Unclear reporting structures for health outcomes in relation to the resources utilised;
- Lack of adequate and effective avenues and structures for complaints handling and citizen engagement at the facilities and oversight structures;
- Unclear insurance schemes for the public including the Kshs. 4 Billion Students insurance plan and other insurance schemes being implemented by different county governments.
Designing Working Strategies for Health Accountability
In view of the need for informed and effective development of working strategies to enhance transparency and accountability in Kenya’s Health Financing models, TI-Kenya would initiate a first round of research on the following areas of interest:
- Enabling Environment: any laws, policies, rules, or regulations, at both a national and county-level, that might impede the effectiveness of the various health financing models.
- Access to Information: the extent to which the identified health financing models are structured towards ensuring attainment of the highest attainable health standards including ensuring equitable, affordable and quality health care to all citizens.
- Public participation: the extent to which public health financing models allow for effective public participation in their formation and implementation including transparency, accountability and feedback mechanisms.
- Value for money: how the various health financing models respond to the need to ensure value for money in provision of services and health resources.
Participants also identified other opportunities and strategies to support realisation of the right to health including:
- Collaborative research, evidence gathering and information sharing;
- Collective action, advocacy and awareness creation;
- Elaborate stakeholder engagements aimed at building consensus and influencing policy;
- Policy reforms informed by the Constitutional provisions on the realisation of the Right to Quality Health Services, Access to Information, Public Participation and Prudent use of Public Resources;
A follow up engagement on this discussion would be called to validate the research results from an initial assessment on the highlighted areas on transparency and accountability in Kenya’s Health Financing Models.

